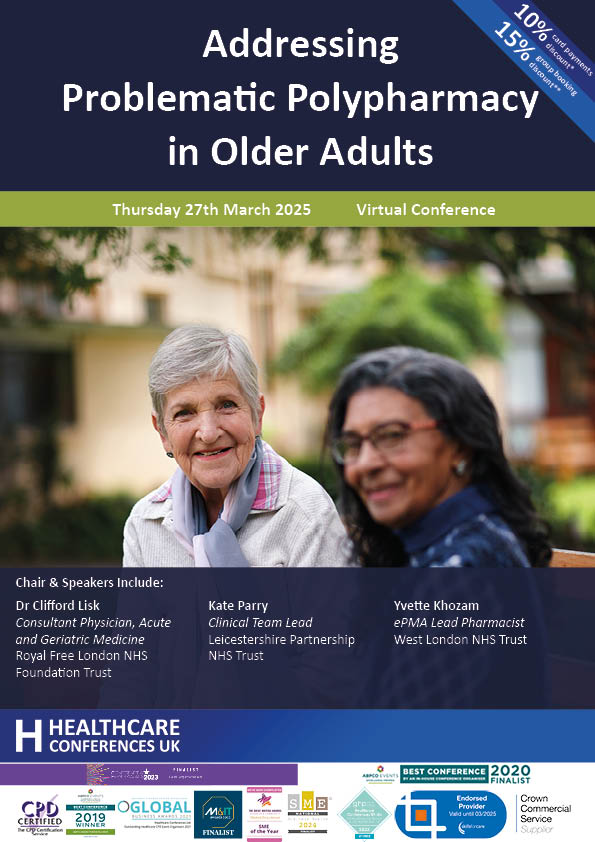
Polypharmacy is a growing concern that requires a multi-faceted approach for effective management. The risks of polypharmacy are significant, but with the right strategies in place, we can mitigate those risks and improve patient outcomes in older adults. This conference will support you to understand the complex issues around problematic polypharmacy and stopping inappropriate medicines safely in older adults. The conference will discuss current issues and trends, support clinicians to identify problematic polypharmacy, develop your skills in leading effective shared decision making structured medication reviews and focus on difficult issues such as discontinuing mental health medications, understand interactions with herbal and dietary supplements and explore strategies for discontinuation syndromes, adverse effects and tapering.
“Problematic polypharmacy adds a cost to the healthcare system and diminishes quality care for the patient – and most of this is entirely preventable.”
Health Innovation Network NHS England 2024
“Polypharmacy, commonly defined as taking at least five drug treatments, is common in older populations. Although older adults are more likely to have multiple chronic conditions, and guidelines often recommend multiple drug treatments, studies have found that polypharmacy can lead to problems such as adverse drug events, drug–drug interactions, drug treatment non-adherence, cognitive and functional impairment, and increased risk of frailty, disability, falls, hospitalizations, and mortality.”
The BMJ May 2024 BMJ 2024;385:e074892
“Overprescribing is the use of a medicine where there is a better non-medicine alternative, or where the use is inappropriate for that patient’s circumstances or is inconsistent with their wishes, and can lead to problematic polypharmacy (a person’s concurrent use of multiple medicines). Polypharmacy may be appropriate for a person with complex or multiple conditions if their medicines are optimised and prescribed according to best evidence. However, it can be problematic when the benefit of the individual medicines is not realised.”
NHS England September 2024
This conference will enable you to:
Network with colleagues who are working to reduce problematic polypharmacy in older adults
Learn from outstanding practice in addressing polypharmacy
Understand common clinical presentations of polypharmacy
Reflect on lived experience and ensure shared decision making
Explore best practice in identifying problematic polypharmacy, understanding which patients and which medicines or combinations of medicines present the highest risk and how the use of polypharmacy prescribing comparators can help
Develop your skills in leading effective shared decision making structured medication review
Identify key strategies for deprescribing mental health medications including those that can cause dependence and withdrawal
Understand which herbal medicines and dietary supplements can be problematic
Develop your skills in managing medicines that have elevated risk during discontinuation through discontinuation syndromes, managing adverse effects and tapering
Support people to better understand the medications that they take
Self assess, reflect and expand your skills in prescribing practice whilst understanding your limits of practice
Supports CPD professional development and acts as revalidation evidence. This course provides 5 Hrs training for CPD subject to peer group approval for revalidation purposes